
Here, we comprehensively cover ketamine in mental health.
To start, please listen to this conversation regarding the guide’s content while you read on…
Next, explore Mad Scribbler’s 7-year journey as a walkthrough and primer below. The guide summarizes the site’s extensive content into a 10-minute read.
Navigate deeper topics using the TOC (≡) and the hyperlinks below, which lead to detailed information with studies, citations, and sources.
Listen by clicking play above each section, which works on most devices. If it isn’t on your phone, try PC. There may be delays to start and during reading as the text is sent to an AI in the cloud to be processed. Please wait a bit.
● Introduction
This site grew from a comprehensive guide on Reddit (r/therapeuticketamine), which u/madscribbler has maintained for several years. The post proved immensely popular with those starting therapy. However, as more was learned about ketamine, the post’s 44000-character limit restricted what could be said.
At this point, collaborators reached out regarding turning the guide into a resource website, which is the site you see today.
We strive to reflect current research and cover the therapy fully. We take great care to cite our sources throughout.
Provide feedback if anything you read conflicts so we can update if necessary.
Below I address questions for those exploring, beginning, or looking to get more out of their treatment. I edit the guide with things we learn, so it’s continually evolving.
In r/KetamineTherapy we are pinned to the top of the sub.


Share us in r/therapeuticketamine under the guidelines per our Community page (along with other subs in our community page or ketamine-related subs), and with friends.
Please also share it with your providers, as many providers use us as a primer for their patients (including Dr. Pruett & Team (at Taconic).
Providers use Request to be Added to Directory.
Please take a moment and give us a quick Provider Rating. We annotate our directory with this feedback for the benefit of others.
We would like to see the site grow even more. If you find it useful, please pass us along to others you know we can help.
Ask questions in the comments, and I’ll incorporate the answers here and respond.
● Authors
This combines personal experience over six years on the therapy, hundreds of conversations with others on Reddit subs, and research where it is available. Without fail, others take issue with some of what’s said here, so I attempt to call out contrasting viewpoints where criticism has been raised.
I specialize in AI and cognitive computer architecture based on neurobiology, neural networks, and big data.
My wife is a doctor specializing in neurological patients, traumatic brain injury & spinal cord injury at a renowned hospital in the discipline.
My provider specializes in ketamine therapy, and I’ve participated in many studies. I’ve been an active member of the ketamine Reddit scene for many years. We recommend you join this sub where we interact the most—r/KetamineTherapy (as we are unrestricted there). Also, join r/therapeuticketamine for community support and a large group of people to relate to.
Multiple site content collaborators all have extensive experience with ketamine therapy, too.
● Resources
We recommend you listen to primarily instrumental music, with very few words, and to make sure any words that are included be positive, uplifting and congruent with a safe, healthy mind space. If you are looking for a good session playlist that will promote a healthy and safe trip, use our curated playlist Ketamine Saved Me (on Spotify).
Education is key in getting the most out of your therapy, and the podcast Ketamine Insights (also on Spotify) has great content on the most recent topics, and new episodes are published frequently. The hosts are well versed in ketamine therapy and bring a lot of good topics up for discussion. When you have time, give it a listen. For an episode where I was interviewed, click “It was a revolution for my psyche”, Rob’s journey to mental health.

● TOC
Below are the sections of the guide linked directly. You will jump straight to what you select. Keep reading below if the first time to the guide.
Introduction
Authors
Resources
Symptoms vs. Results
Treatable Mental Illnesses
Effectiveness by Mental Illnesses
Treatment Center
Administration
Bioavailability
Half-Life
Experience
Transliminal Space
● Symptoms vs. Results
I am BP1, with psychotic features. I struggled with persistent bipolar one depression, which did not respond to SSRIs, constant (daily) ideation with extensive planning, and complex psychological issues such as self-persecution complex and complex PTSD.
One trigger resulted in PTSD maladaptive behavior that would trigger another, which then triggered again until the first trigger was reached again. Round and round it went. This resulted in significant mood instability, anger at inappropriate times, paranoia, a general suspicion of others being out to get me, inferring hidden agendas, and a feeling of complete hopelessness. I undermined my successes through self-persecution because I subconsciously didn’t feel I deserved them.
I was choosing untrustworthy people to surround me, which led to many traumatic life situations, making them worse and worse over time.
I would ruminate on negative thoughts, situations, and feedback in a cycle of unhealthy self-talk. I saw the world through a very unhealthy lens, reinforcing all the fear and paranoia. I couldn’t feel joy or happiness, for those led to self-defeat, so I was wired entirely wrong.

I’ve been on ketamine for six years. I have had 100% remission of rumination, depression, ideation, CPTSD, and almost all trigger situations non-stop. Ketamine has rebuilt my healthy synapses, neurons and relocated dendrites, so I can happily cope with life and now view the world through an objective lens showing love, support, compassion, and acceptance of me and who I am today.
Ketamine improves cognition, memory, and mental flexibility, so damage caused by depression has been healed completely. This results in mental clarity and an overall ‘lighter’ feeling. Depression was a heavy blanket that weighed me down, unmotivated. Hard to start and harder to finish. Ketamine made my mind quieter; I no longer cycle on intrusive thoughts. I am no longer obsessed with suicide. I no longer ruminate. Look to this page to see how ketamine improves the default mode network in our mind, quieting it and taking away cyclic or impulsive thoughts completely—the inner narrator quieted in my mind, which feels tranquil.
I love life and live every minute. I feel joy and happiness now, and I’m very content almost all of the time. These past six years have been the best of my life.
I knew ketamine was working for me with the first dose (no more ideation after the first dose). The depression lifted in the first few doses. Once the healthy synapses grew, I reinforced them. As I was triggered, I broke down trauma underneath and differentiated it from my new reality, rewiring them to no longer fire. Six + years in, I’m a completely different person that loves life in every way, and ketamine has been so successful I don’t feel like any other treatment is needed to feel better.
Being bipolar, I maintain a mood stabilizer, antipsychotic, stimulant, and sleep med, but I no longer need recreational drugs and several prescriptions I used to take.

It takes ketamine time to regrow synapses and relocate dendrites depression and PTSD Maladaptation creates. So, like many, I did feel worse before I felt better.
See: Feeling Worse When Starting Treatment
Emotional processing is complicated, significantly before the depression lifted and the new synapses developed and grew strong. They’re like muscles, and they need exercise to grow strong. So, the therapy was complex emotionally at first, and I cried a lot. Profuse sobbing. It was so cathartic though. To release all that lifted the weight of the world from my shoulders.
So, in summary, ketamine lifts rumination, depression, and ideation completely, and words can’t describe how good that feels. Incredible feeling. It also restructured my brain to appreciate these things and come healthily to the world.
I’m so happy now, consistently happy and healthy.
It’s why I wrote the guide and built the site. Ketamine made such a difference for me I’m getting the word out to everyone that it can help.
● Treatable Mental Illnesses
Ketamine is indicated for treating Bipolar 1 & 2, rumination, depression (such as major depressive disorder and treatment-resistant depression), PTSD & CPTSD, substance abuse, persistent anxiety, intrusive thoughts, Alzheimer’s & Dementia, Autism (ASD), ADHD, Borderline Personality Disorder, Panic Disorders, suicidal ideation and self-harm, and OCD. Most of the benefits are reported by patients and doctors, so few studies exist to prove out benefits, although more come out every day. We’ve taken great care to cite our sources across the site and add new content every week.
Spravato has been proven effective and is FDA-approved for treatment-resistant depression (TRD) only (in clinical trials). Racemic ketamine is off-label for mental health purposes.
While ketamine has a long history as an anesthetic and painkiller, I don’t cover chronic pain or anesthesia in the guide. There is a supplemental page on neuropathic pain here. We are focused mainly on the use of ketamine therapeutically, be it do it yourself or through a provider.
Ketamine is not considered the first line of defense, so some mainstream healthcare guidance is to try first-line antidepressants first. Given how effective ketamine is, I would use it as the first option, but the medical community is conservative.

If other antidepressants haven’t worked or cause unwanted sexual side effects (which is common), or you want to go straight to the best option IMHO, explore ketamine.
Ketamine has been proven in treatment-resistant depression, which requires multiple antidepressants to be tried first to indicate by most evidence-based practices. Do not self-diagnose. Only do diagnosis through a qualified health provider.
See: Treatable Mental Illnesses
● Effectiveness by Mental Illness

This is the result of our 30-Second Survey, current as of the end of last week. This is patient-reported effectiveness.
If you haven’t completed the survey, it takes less than 30 seconds. It is very helpful for us in various ways, providing the results below and evidence to use in media to overcome ketamine’s stigma. Ketamine for mental health regularly gets poor press coverage.
In the survey, we identify non-responders as they reported scores lower than or equal to two stars or less for overall effectiveness. The non-responders skew the overall scores downward so pay attention to the number in each category. The resulting effectiveness % is calculated using those who responded and scored higher vs. those who did not respond.
Categorically, we’ve observed that there is a direct correlation between the time on the treatment and the patient’s success. The longer someone has been treated, the higher they tend to score on the survey. This underscores the need to stick with it even when you feel worse at first for the best results.
Effectiveness Rating Legend
Amazing | |
Highly Effective | |
Effective | |
Partially Effective | |
Ineffective | |
Not Rated (No Submissions Yet) |
Survey Results
Overall Effectiveness of Ketamine Therapy | 135 Surveyed, 15 Ineffective (88% Effective) |
Average Months on Treatment | 10 Months |
Major Depression Disorder (MDD) | 86 Surveyed, 10 Ineffective (87% Effective) |
Mood Instability | 54 Surveyed, 7 Ineffective (88% Effective) |
Suicidial Ideation | 51 Surveyed, 7 Ineffective (86% Effective) |
ADD/ADHD | 34 Surveyed, 8 Ineffective (76% Effective) |
PTSD/CPTSD | 58 Surveyed, 7 Ineffective (88% Effective) |
Triggers | 41 Surveyed, 6 Ineffective (85% Effective) |
Treatment Resistant Depression (TRD) | 58 Surveyed, 7 Ineffective (88% Effective) |
Anxiety | 78 Surveyed, 8 Ineffective (90% Effective) |
Intrusive Thoughts | 53 Surveyed, 11 Ineffective (79% Effective) |
Rumination | 58 Surveyed, 9 Ineffective (84% Effective) |
Substance Abuse | 27 Surveyed, 2 Ineffective (92% Effective) |
OCD | 15 Surveyed, 3 Innefective (80% Effective) |
Personality Disorders | 14 Surveyed, 3 Ineffective (78% Effective) |
Panic Disorders | 35 Surveyed, 4 Ineffective (88% Effective) |
Psychosis | 4 Surveyed |
Anger | 11 Surveyed, 1 Ineffective (90% Effective) |
Schizophrenia | 4 Surveyed |
BP1 | 7 Surveyed |
BP2 | 14 Surveyed, 1 Ineffective (92% Effective) |
Autism | 9 Surveyed |
Alzheimer’s | 4 Surveyed |
Thank you; every submission adds weight to our collected evidence!
● Treatment Center

Treatment is done via ketamine clinic often, and telemedicine is an alternative. There are practices everywhere that specialize in ketamine.
Search Google for ‘ketamine providers near me’ or ‘ketamine telemedicine providers.’
Our site hosts a comprehensive provider directory, with a matrix by state in our Providers by State page.
With a clinic, expect a $350ish consult fee. Most do IVs, often $300ish to $700ish each, and standard practice is 6 to 8 IVs administered over two to three weeks. Telemedicine and some clinics also do troches (sublingual lozenges). Troches, by comparison, are $75-$90 for the equivalent of 4 IVs.
More costs can be found in costs by route of administration.
Make sure your treatment center believes in patient education and patient self care. It’s key to know the dosages you are being given, and at what frequency.
Ketamine increases anesthesia tolerance across the board – so if one were to be in an ER, and about to undergo surgery they’d need to tell the ER what dose of ketamine they take, and at what frequency for the anesthesia to be adjusted appropriately (upward).
As I understand it, worst case scenario is you could be in emergency surgery and not sufficiently sedated – iow, sedated enough to be paralyzed, but not sedated enough to be unconscious. And then experience the surgery.
Which is unlikely I’m sure, but I know when I went in for a colonoscopy and gave them my doses and frequency they doubled the anesthesia. So definitely a remote possibility.
Many patients share the guide with their providers, and as a result are able to have more in-depth conversations with their providers about their course of treatment, the potential side effects, and other related concerns. Be sure you choose your provider carefully, and that you are well informed and educated about your treatment, and related protocols.
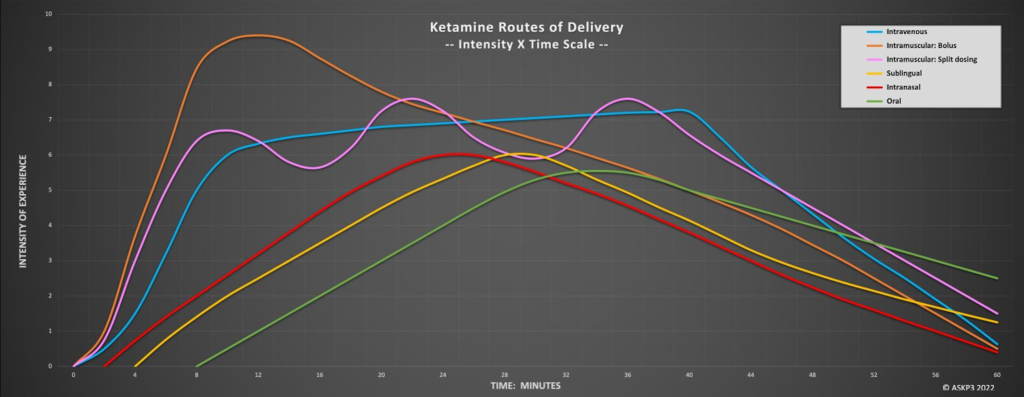
● Administration
See: ROAs – Routes of Administration
The clinic can administer ketamine using varied routes of administration. Most often used are IVs, but there are IM injections, nasal spray, troches (aka lozenges), pills, rapid dissolve tablets, suppositories, transdermal, and nebulization. Telemedicine often uses troches or rapid dissolve tablets as they ship better.

Typically, an IV series is done over two to three weeks, with injections Monday, Wednesday, and Friday, over two/three successive weeks, for example. This initial series of 6-9 (typically) infusions are called the “loading doses“.
I started with troches, did them for two months, then did my IV series of 6. I use a local provider overseen by a psych specialized in ketamine. I know many choose telemedicine, and there are several viable alternatives, however, do your research, as several get many bad reviews for poor support during the treatments. If we see enough negative feedback about a provider, we will annotate our provider directory to call that out.
At first, in my treatment, I found troches preferable to IV. No injection was involved. I could do them as I saw fit, go as deep for as long as I liked, and ensure I had a quiet, safe space for the experience. It’s essential to be in a safe space with limited (no) interruptions (outside of a friend/therapist, perhaps). Still, while you’re under the influence, you’re vulnerable, and avoiding trauma is essential (I’ll go into that more below).
Do not mix ketamine with water, like a bathtub, hot tub, or pool. Cognition can take a break while under ketamine, and drowning is a risk. Instead, find a comfy recliner, couch, or bed. It is anesthesia, and you will fall unconscious if the dose is too high.

Another reason I preferred troches to IV is because clinics do o2 stats and blood pressure checks, which negatively interrupt the experience – so you’ll be knee-deep in childhood trauma, and a nurse will bug you. Not ideal. If this is your provider’s practice, ask them to limit their interactions to before and after the dose is administered and has been completed. My practice changed its standard operating procedure for everyone upon this request.
In the IV series, dosages are increased over the series to promote higher dissociation. This can be done with troches. However, heed the warning above, and please read carefully about the dosing below because more is not always better.
With IV administration, you can request magnesium alongside, which increases the effect and reduces hangover.
Ketamine can cause nausea in some people, so they can also administer Zofran, an antinausea drug.
You can supplement it with magnesium glycinate using troches or other non-IV methods. It is highly bioavailable and comes without the laxative effect of magnesium l-threonine. 400mg. An early morning dose on the day of your ketamine is recommended, although magnesium is good to take at 400mg daily.
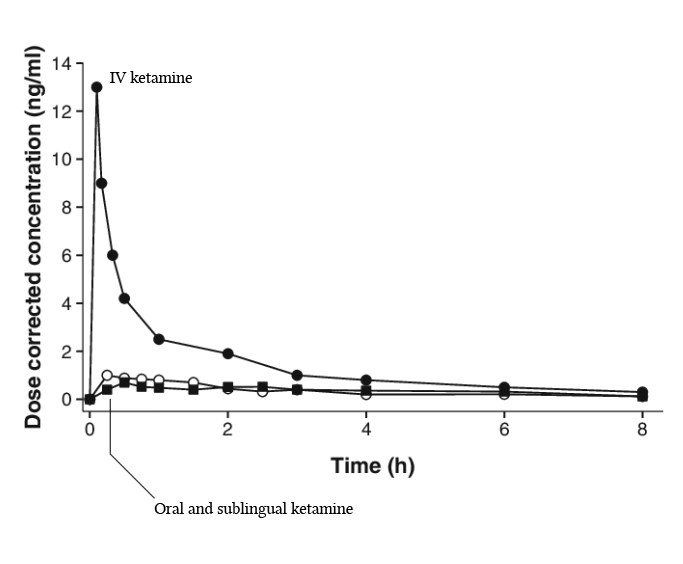
● Bioavailability
Different routes of administration have differing bioavailability levels, which translates to more highly effective doses at lower comparative ketamine doses, which can help prevent bladder harm, covered last in the guide. More detail there.
With troches, try and keep the saliva in your mouth, under your tongue, as much as possible. Ketamine is more bioavailable when absorbed through 1st pass digestion via mucosal membranes. See Spit or Swallow Oral? When you swallow, ketamine goes through second-pass digestion via the liver, giving you more of a hangover (dull headache and fatigue for 1-2 days afterward) and increasing bioload over other approaches. Given we all have a natural swallow reflex, troches are bound to end up in the stomach to a degree regardless. But if you hold the spit in your mouth as long as possible (ideally 45-min, to 1-hr) and then spit the ketamine out, you’ll have little hangover compared to swallowing.
Generally, oral administration of ketamine has a relatively low bioavailability, typically around 20%. This is due to the extensive 2nd-pass metabolism in the liver, where a significant portion of the drug is metabolized before it can reach systemic circulation.
Some patients have reported that their oral mucosa will be affected by troches and RDT’s, causing inflammation and potential shedding of the inner lining of the cheek. This, like the bladder, will heal completely over time.

In regards to tooth enamel:
- Ketamine is acidic, with a pH of 3.5-5.5. Acidic substances below the critical pH of enamel (5.5) can erode enamel over time.
- However, the limited contact time with low concentrations used therapeutically is unlikely to cause significant enamel erosion.
- One study found no difference in salivary pH after intravenous ketamine administration. No clinical studies have directly evaluated the effects of long-term therapeutic ketamine use on dental enamel.
- Proper oral hygiene practices should prevent any minimal erosive effects of therapeutic ketamine use.
Overall, while more research is needed, there is no strong evidence currently that therapeutic ketamine under proper medical supervision degrades or erodes tooth enamel to a significant degree, especially with short-term use.
The nasal is even better at 1st pass digestion than under the tongue (more mucosa), resulting in a higher bioavailability than sublingual.
Intranasal administration of ketamine, by way of comparison, has a higher bioavailability of around 45-50%. This is because intranasal administration allows the drug to be absorbed directly into the bloodstream through the mucous membranes in the nose, bypassing metabolism in the liver.
You may want to consider getting a nasal dispenser. This can lower the risk of bladder damage, covered last in the guide. See Vitality Medical to Buy a Nasal Dispenser.
Racemic rapid dissolve tablets and racemic troches can be placed into warm saline, dissolved, and dispensed nasally with this device.

The suppository also has higher bioavailability than the sublingual due to more mucosa. Here, follow the same protocol to prepare RDTs or troches and inject rectally with a rectally appropriate syringe.
Suppositories generally avoid first-pass metabolism like nasal, IV, and IM. Suppositories can have variable absorption depending on the specific formulation and individual differences in absorption in the rectal mucosa. It is generally thought to be higher than oral, however.
So, all that said, always involve and follow your provider’s guidance in any variation to your prescribed treatment plan, including formulations and route of administration. Discuss any changes with them, and get approval to try a given technique. You need to understand your provider’s protocol for such approaches and protocols for infection mitigation.
● Half-Life
The half-life of ketamine is 2.5 hours. Ketamine takes down fine motor controls, making driving, operating machinery, and other tasks requiring coordination difficult.
If pulled over or in an accident and tested immediately after dosing – for example, immediately after an IV, you will be given a DUI. Ketamine can be a false positive for PCP.
Waiting 24 hours to drive brings the ketamine down to nearly non-existent levels.
If doing in-office administration, we recommend a designated driver. Many providers require this.
Here are the key points about the half-life and driving recommendations for ketamine used therapeutically:
- Ketamine has a relatively short half-life of around 2-3 hours. This means that after 2-3 hours, the plasma concentration of ketamine is reduced by half.
- However, the psychoactive effects of ketamine typically last 45-90 minutes when used at therapeutic doses. The effects wear off gradually.
- Ketamine is metabolized into norketamine with a longer half-life of around 12 hours. Norketamine is also psychoactive and can prolong the effects.
- Most guidelines recommend waiting 24 hours after using a therapeutic dose of ketamine before driving or operating heavy machinery. This allows time for the drug and metabolites to be sufficiently cleared from your system.
- Some experts say waiting 12-16 hours may be sufficient based on the short half-life, but 24 hours is a more conservative timeframe given the presence of active metabolites and individual variability in response.
- The effects of ketamine vary significantly between individuals based on factors like body size, liver function, other medications, etc. It’s best to be cautious when judging your ability to drive safely after ketamine.
- If you must drive sooner than 24 hours, be careful and attentive. Have someone else drive if you notice lingering effects like sedation, slowed reflexes, coordination issues, or altered judgment. Please don’t take any risks when it comes to driving safely.
In summary, a 24-hour wait is recommended after a therapeutic ketamine dose, but if driving sooner, take every precaution and avoid driving if any effects persist. The clearance time can vary.
● Experience
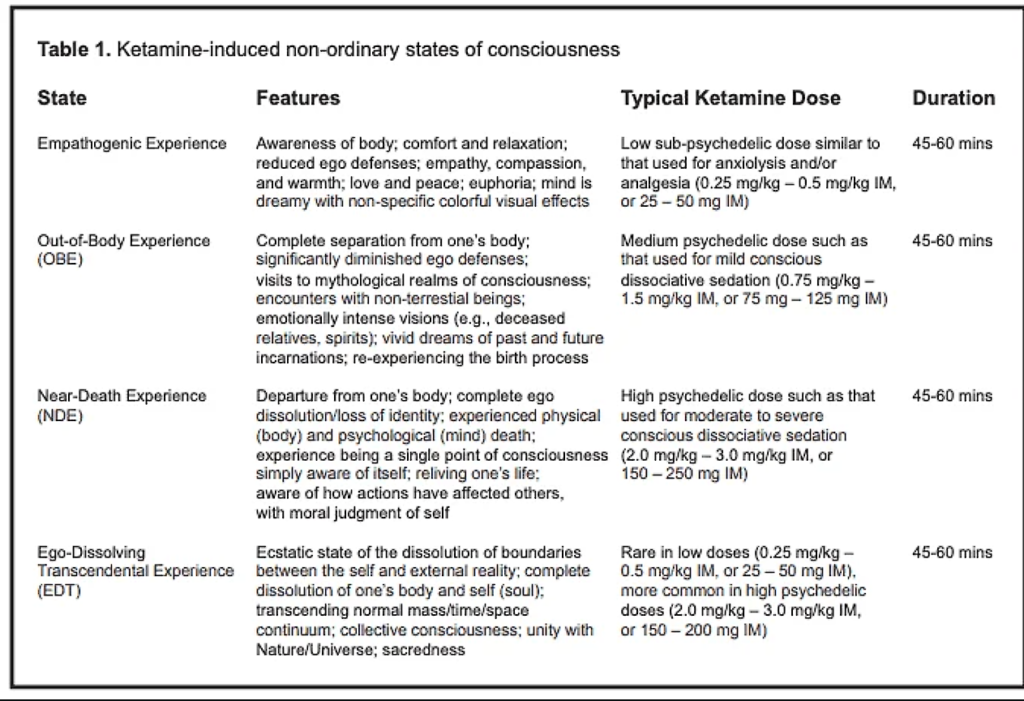
See: Non-Ordinary States of Consciousness
See: Disassociation
See: Preventing Panic
See: The Transformative Power of Ketamine
Reports of experience range from trivial effects to profound insight into trauma and unhealthy mental patterns, complete in-situ deaths, and reincarnations (rebirths/near-death experiences), communing with higher consciousnesses, and a complete loss of comprehension/cognition. Some report reality collapses to a single infinite point, then rebuilding based on Mandelbrot fractals (this can be the experience associated with a k-hole). Generally, however, the experience of ketamine is described as ineffable.
This is dose-related. There are benefits to various states of dosing, which I will cover next.

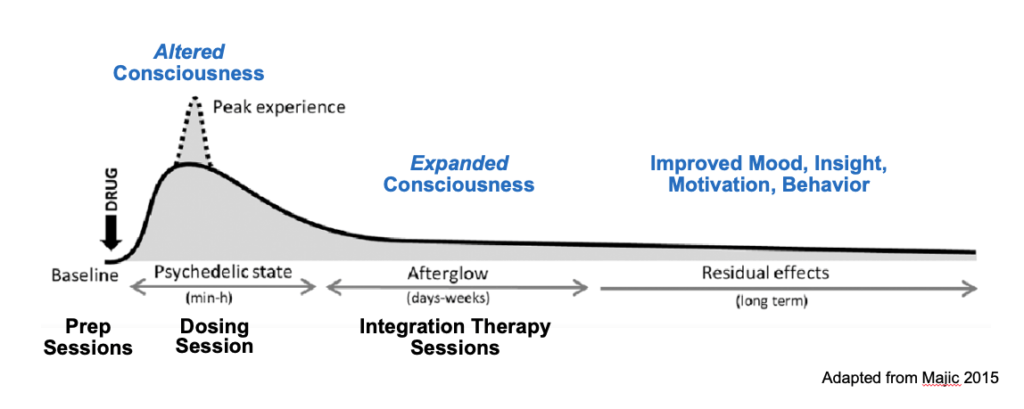
To start, ketamine disables the perineuronal net, a protective system in the brain dealing with trauma. This is one of its greatest strengths, as by disabling the net, the mind becomes adaptable to how trauma is stored and the stimulus-response patterns of triggers. This comes with some risk, though, as when new trauma occurs within the window wherein the net is down, the trauma won’t be processed as normal, and the effects of that are unknown. Due to this, my advice is to avoid traumatizing yourself with the experience itself.

Disassociation is accomplishable via a moderate dose, so there is no need to wipe out your cognition (anesthetic dose) or ‘ego-die/khole‘. Some report therapeutic value in ego-death levels, and some research indicates reset of brain circuits and neural networks at those doses can be therapeutic. I have dosed at elevated levels and found benefit in understanding myself spiritually, yet there is some risk to my sanity. Know, however, that those doses are not required for ketamine to be effective, and they can be traumatic if you aren’t prepared for them.
Again, my guidance is to start low and work up. Trauma processing is best when your ego is present and lucid, which is lower doses than ego death. Start low and work up to it if you want to go as far as ego death. As you’ll see below, though, many of ketamine’s therapeutic aspects do not require this.
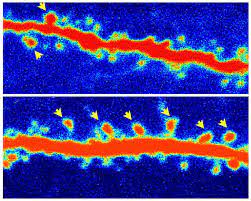
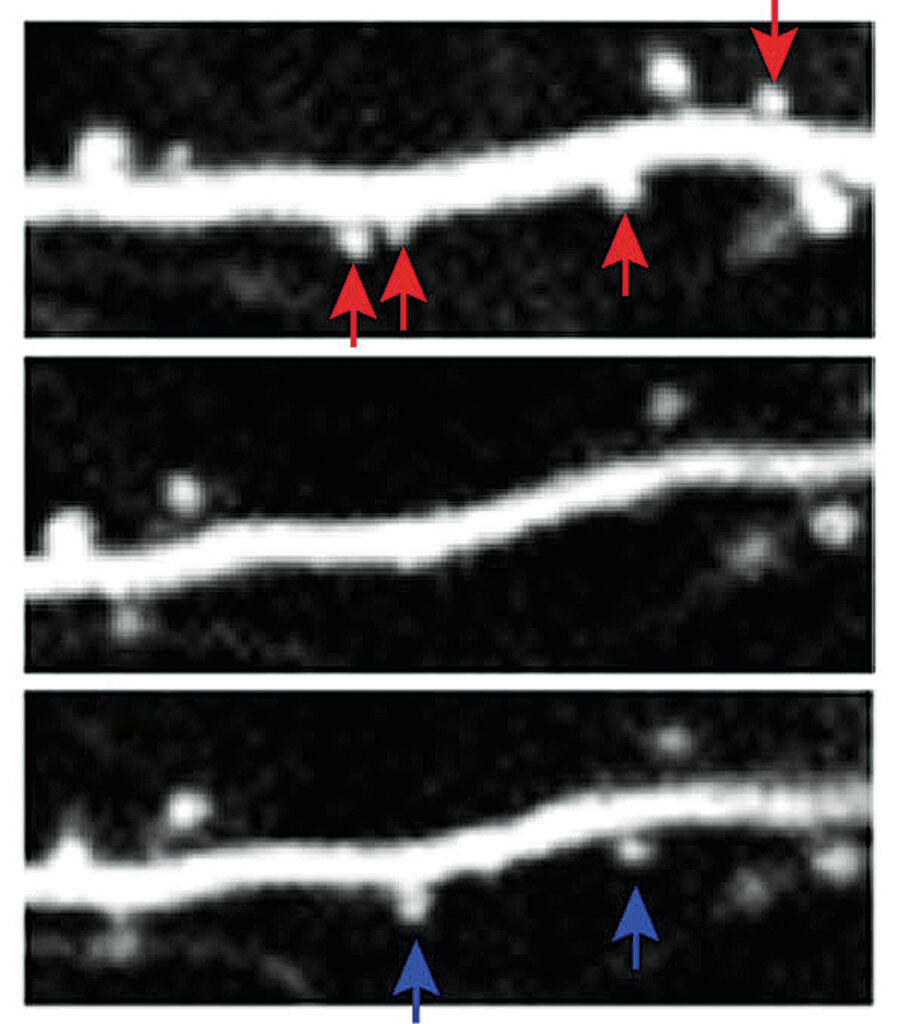
Ketamine at high doses recycles neural networks/resets brain circuits (aka neural fragmentation), so you may be out of it for a bit. Do not let it concern you — it’s a natural and transient part. Try not to go this high, but know it happens, and nothing to worry about. For more about this, you can read this Sheep on K for a good study. Research has shown the human brain doesn’t behave precisely similarly, but it should give you the gist.

See even more of Ketamine’s Action in the Brain.
Note that the flatlining of brainwaves shown is hypothesized to create a Near Death Experience (NDE) for some while undergoing the experience.
Again, trauma processing only requires a moderate disassociated dose. This keeps you mentally intact but opens memories from suppressed traumas and will surface the issues your mind needs help with. At these doses, ketamine exposes suppressed memories, triggers (stimulus/response), traumas, and thought patterns for modification. This is how it most effectively treats PTSD & CPTSD. At these doses, the recall on ketamine will be near perfect.
Dissociation provides new perspectives on problems, memories, and triggers — and each time you take ketamine, the view differs. This will give you much to think about and work on.
Do not try to make your mind focused. It will prove difficult. Trauma is processed in the background; you need not work on it consciously. You can, though, and as you understand triggers better, you can target them intentionally and rewire them to fire appropriately.
Ketamine collapses neural networks/brain circuitry and some brainwaves in no particular order and to varying degrees while enhancing other neural networks/brain circuits/brainwaves. This is a highly active field of study, with imaging of all nature being produced, and the terms are broad because there isn’t consensus on the exact mechanisms here.
See: Brainwave Changes

As a result, ketamine is unpredictable in that the same two doses will rarely have the same effects. Each time you take ketamine, the subjective experience and the nature of the trip will vary – some trips will be more vital and more profound, while others may not even induce visual or any mental effects. Each time you take ketamine results in a new point of view, however, and part of that variability is thought to stem from the variations in these collapses and resets. Again, theoretical.
Like many, I did feel worse before I felt better. Processing trauma was brutal, and I cried non-stop for a couple of days after each dosing for the first eight or so.
See: Feeling Worse When Starting Treatment
By starting with troches, I had already begun the formation of the new synapses and dendrites found in a healthy brain. I had pre-processed a lot already going into the IVs, so my IV series was anti-depressive and healing.
Those starting with IVs build the new synapses and dendrites with the first dose, and the growth happens 12-72 hours after a dose. In the beginning, the newly formed structures are weak and need a lot of reinforcement. The series of 6 IVs gives them lots of time to build out, and what you do during your series can affect how well they build out, and like a muscle, they need exercise. Do everything you can to be healthy. Therapy, yoga, walks, meditating, bonding with loved ones, processing emotions, letting them come and go. Learn mindfulness. This is key, and being present now is what gets rid of triggers.

Now is different than then. Always remember that.
Often people who are in the first few IVs wonder, “Is this even working for me” “I’m discouraged. This is my last hope, and I need it to work for me”, and “Am I doing it wrong?”. No, you’re not. It takes time to regrow and adapt to using the new neural networks. You can’t force it, and there are no ‘mistakes’ you can make that will change the course of action.
In the first few doses, a lot of pent-up emotion is released, and you don’t have healthy neurons online to cope quite yet. So, it’s discouraging for some. It’s common Feeling Worse When Starting Treatment. They are processing many emotions, are still depressed, and wonder if they should continue therapy. It’s expensive and makes them feel like crap, so why keep doing it?
That is when you need to keep going because your brain is still healing, and the depression hasn’t lifted yet. Keep with it, and as your mind recovers, you’ll feel better. At a minimum, do the first 6 IVs, but it might take more, and in my case, I went to monthly boosters and did that for three years to reinforce the synapses and to remain open for processing.
Even though the first few doses may be difficult emotionally, your ideation (should you have any) will be removed with the first dose, so you won’t want to end your life. If you continue to ideate after the first dose (which happens rarely), it’s a sign of cyclic ideation caused by depression and may take a while longer to resolve as your networks build.
● Transliminal Space

The term “transliminal” itself is derived from Latin, where “trans-” means “across” or “beyond,” and “limen” means “threshold.” So, “transliminal” in this sense is to be interpreted to mean “beyond the threshold.” In a psychological context, this refers to experiences or states of consciousness that go beyond ordinary, everyday awareness.
Transliminal space is the boundary between awake and in a dream state at the edge of anesthesia. It can seem as if you exist solely of mind alone in the void and of a completely separate and transiently invisible physical body.
There are theories that transliminal space, at moderate doses, is a sweet spot for deep introspection and is the most therapeutic level. I cover doses below in more detail, but in my experience, when transliminal, I feel I’m merged with the higher mind and that it’s teaching me more from which I can grow – if in no other way than a much deeper understanding of myself.
● Near Death Experience (NDE)
Many people who k-hole see that event as a near-death experience. This can feel like an in-situ reincarnation. An NDE is characterized by the following:

It’s important to note that not everyone with a near-death experience will experience all of these elements, and the experience can vary greatly from person to person. The interpretation of these experiences can also be influenced by a person’s cultural and personal beliefs.
- Out-of-Body Experience (OBE): This is often the first element of an NDE. The person feels as though they have left their physical body and are observing events from a detached perspective.
- Tunnel Experience: Some individuals report moving through a dark tunnel or void, often towards a source of light.
- Feelings of Peace and Joy: Many people report feelings of profound peace, love, and joy during an NDE. They often lose all fear of death.
- Light: Individuals often report being drawn towards a bright light. This light is often described as being of unearthly brilliance and warmth.
- Encounter with Others: Some people report encounters with deceased loved ones or spiritual beings. These beings often communicate with the individual, offering comfort or advice.
- Life Review: Some individuals experience a rapid, panoramic playback of their life or portions. A sense of profound understanding or insight often accompanies this.
- Reluctance to Return: Many individuals who experience an NDE are reluctant to return to their physical bodies and earthly life. They often report a sense of disappointment when they revive or are resuscitated.
- Transformation: After an NDE, individuals often report profound changes in their attitudes, beliefs, and values, including a decreased fear of death, an increased sense of purpose and self-worth, and a greater concern for others.
● Out of Body Experience
An out-of-body experience (OBE) is a phenomenon in which a person perceives the world from a location outside their physical body. This experience can vary greatly from person to person, but there are some common elements that many people report.
- The feeling of Separation: The individual often describes a sensation of being able to view their physical body from an external perspective, as if they have separated from their body and are observing it from a distance. This is often described as looking down on their body from above, but the perspective can vary.
- Altered Perception of the Environment: The environment during an OBE may appear similar to the normal physical world but with subtle differences. Some people report that the world seems more vivid, with colors appearing more vibrant. Others describe the environment as being dreamlike or surreal.
- Sensations: Various physical sensations may be associated with OBEs. These can include feelings of floating or flying, spinning, or rapid movement. Some people also report a sensation of vibration or buzzing as they separate from their body.
- Emotional Responses: The emotional response to an OBE can vary widely. Some people find the experience exhilarating or profound, while others may find it frightening or disorienting.
- Return to the Body: The return to the body is often described as a quick or instant process. Some people report a sensation of being pulled back into their body, while others describe simply finding themselves back in their body without a clear transition.

It’s important to note that OBEs are often associated with altered states of consciousness, such as near-death experiences, deep meditation, psychedelic substances, or certain sleep states. However, they can also occur spontaneously without any apparent trigger. The exact cause and nature of OBEs are still subjects of ongoing research and debate in the scientific community.
● Super-Hearing

Ketamine disables the perceptual filters your mind uses to filter out background noise. So, when you’re on ketamine and not listening to something like music, you may hear sounds you have tuned out automatically all the time, like the furnace or air conditioning.
Take this as an opportunity for your ketamine self to be kind to your future self. If doing at-home treatment, find all the little rattles and creaks while on ketamine, and your life will be far quieter around you afterward.
For example, I found chattering glass vases when the air conditioner was on. I appreciate the difference now that low-level background noise is gone, having silenced it.
● Neurological Growth
● Improved Cognition
● Neural Plasticity
See: Brain Changes
See: Neural Networks
See: Neural Plasticity
See: Memory
See: Perineuronal Network
See: Neurogenesis
See: Synaptogenesis
See: Dendrite Remodeling
Ketamine has been shown to improve cognition (memory, processing speed, and cognitive flexibility) across correlated studies. For 24-72 hours after a dose, there may be reductions in cognition – however, after seven days, there are marked, measurable improvements over baseline.

Ketamine promotes (at least) three mechanisms through which your brain changes and heals: Neurogenesis, synaptogenesis, & dendrite relocation, regrowth, and extension (aka remodeling).
Ketamine appears to increase the proliferation and development of new neurons from neural stem cells. It does this primarily by activating the mTOR (mechanistic target of rapamycin) pathway, which stimulates synaptogenesis and growth of new dendrites on developing neurons. Ketamine also seems to increase levels of BDNF (brain-derived neurotrophic factor), an important neural growth factor. The most prominent growth occurs in the hippocampus.
Research shows that ketamine rapidly increases synaptogenesis in the prefrontal cortex and hippocampus. It does this in several key ways:
- Ketamine increases brain-derived neurotrophic factor (BDNF). BDNF supports long-term potentiation – the strengthening of synapses based on patterns of neural activity. BDNF facilitates synaptic plasticity.
- Ketamine also activates the mTOR pathway. mTOR signaling promotes the translation of synaptic proteins needed to produce new synapses.
- The new synapse formation induced by ketamine occurs via the rapid synthesis of synaptic proteins like PSD-95, glutamate receptors, and synapsin. This leads to increased density and function of synapses.
- Ketamine also increases the number of mature mushroom-shaped dendritic spines, the sites where synapses form. This further enables synaptogenesis.
Dendrite Relocation, Regrowth, and Extension (Remodeling) –
- Ketamine increases brain-derived neurotrophic factor (BDNF) levels, which promotes dendritic remodeling and motility. BDNF activates pathways that allow dendritic spines and branches to become more mobile.
- The increased dendritic mobility induced by ketamine leads to elongation and branching of dendrites. This allows dendrites to sample a greater area to form new synapses.
- Ketamine also rapidly increases the turnover of dendritic spines, with the loss of certain spines and the growth of new ones. This reorganizes the dendritic network.
- Advanced microscopy techniques have shown dendritic spines redistributing within 30 minutes of ketamine treatment in rodent models.
- The new dendritic configurations allow neurons to form novel circuits and increase synaptic connectivity.
Inducing rapid relocation and rewiring of dendrites, ketamine can quickly remodel communication between neurons in brain regions involved in depression. This may help “reset” circuits that have become dysfunctional, restoring neural plasticity. The reconstitution of neural networks via dendrite reorganization is likely a key mechanism underlying ketamine’s robust and sustained antidepressant effects.
Note that Spravato has not shown the same effect. Again, this implies not rebuilding synapses as effectively, but speculative and not proven through research.
Neural plasticity opens during a dose and persists up to 72 hours afterward. Neural plasticity means your mind is open for conscious modification, and it’s as if your conscious and subconscious can discuss things and come to terms with one another.
Decide to change, accept, and love something; it will become solidified in your mind after the window closes. For instance, you can quit a substance and wake up the next day, not craving it.
The uses of this are manyfold, experiment and surprise yourself!
There is limited research available, but ketamine is also remarkably similar and thought superior to modern treatments for Alzheimer’s as well. Out of five hypothesized pathways for Alzheimer’s, ketamine shows improvements in four and uncertain effects in a fifth.
One of the leading theories in Alzheimer’s is that the dendric spines become complex and, as a result, require expensive metabolic processing. Ketamine reforms dendric spines, making them leaner and more efficient and attaching them to new locations on the synapses. This reduces the metabolic expense of the dendrite and is theorized to act as a precognitive agent against Alzheimer’s. I’ll add more info here as studies proceed.
See Alzheimer’s Disease for more recent updates here.
● Metacognition

Ketamine installs metacognition in that you’ll have a new voice in your head of an inner moderator. It will monitor your interactions and will let you know when you’re in triggered situations so you can resolve those triggers interactively. It will recognize when you are triggered, so you can take those situations into ketamine sessions and work through their underlying pattern. You then will take time to differentiate your new reality from the reality that caused those triggers. Then, in the window of neuroplasticity 12-72 hours post-session, you reprogram yourself to become immune to those circumstances in the future.
It takes time and practice, but this increased capability of your mind to recognize and work through this is called metacognition. Metacognition means greater self-awareness of your mental state, thoughts, and emotions.
Do not be alarmed by this new self-awareness; you will grow into it.
● Fight or Flight Mode
When a traumatic event happens, we imprint the most effective response for “defending ourselves” as a pre-programmed behavior. The pattern forms a “stimulus” that results in an immediate, non-conscious without thought to the response.
We have two nervous systems, the parasympathetic and the sympathetic. The sympathetic system is our “fight or flight” mode, where when it kicks in, it quickens reflexes by reverting to our reptilian brain, which can move limbs more quickly.
The reptilian brain short circuits the cerebral cortex, taking us from our normal, reasonable, well-planned responses into a robot acting out, often in the most inappropriate way. Because circumstances now seem similar enough to the trauma, your reptile brain decided it was the boss and is acting out based on maladaptive coping mechanisms formed in the past.
Recognizing that dynamic, wherein you aren’t conscious of the response, and upon review, it seems highly suspicious of how you responded being inappropriate, is a trigger you’ve identified and need to work on.

● Name Your Minds
Key to ketamine therapy is understanding that there are many minds within oneself, some effective in current-day life, some maladaptive wherein they “worked” in some traumatic situation.
Some examples are the “wise mind,” where responses are well thought out, unrushed, and come naturally. This is our “best” self.
Another mind is the paranoid mind, which explores every dark path to see what the ‘worst case scenario’ might be – just in case so that we can be prepared for it. You know the adage, “Hope for the best, prepare for the worst…”.
That mind stems from my survival instinct, which serves no purpose in modern-day life. Life rarely works out in the worst-case scenario, so I don’t want to carry all that negativity. So I tell that mind to please quiet itself whenever it speaks up. I do not need it.
Other minds could be clever, empathetic, optimistic, or pessimistic. Use your imagination. We all have many.
Encourage healthy minds and discourage your unhealthy ones.
Just speak to yourself inside, and when programming your mind, speak to it in your internal voice. Your executive center controls which mind speaks and which coping strategy gets used when (in the absence of a trigger kicking in the reptilian brain), so tell yourself what you want those minds to do, then remember and reinforce that. This is most effective when you reinforce this when you’re within the window of neural plasticity.
● Deprogramming Triggers

One of the most effective uses of ketamine is removing triggers from your psyche. Once identified, you can analyze and identify the origin of a trigger. Identify the circumstances around when the trauma/stimulus formed and what coping mechanism you developed as a byproduct.
Often, these coping systems are maladaptive and, thus, inappropriate for any given situation. Unfortunately, since they’re invoked as part of the stimulus-response (reptilian sympathetic nervous system), you have very little, if any, control over when they come out. Reason takes a backseat when you perceive something as a threat.
This makes one volatile, often acting inappropriately in various situations.

Find the root, and repeatedly (like a mantra) tell yourself, “Now is different than then!” In the window of neural plasticity, your brain can be rewired to see today’s circumstances as an entirely different scenario, keeping the trigger from firing in the future.
In my therapy, I use my puppy dog as an anchor to the now. She wasn’t around when the triggers were formed, so I mindfully interact with her, hugging her and getting puppy kisses, thus rewiring my stimulus-response system to recognize her as a differentiator when looking to fire triggers. If she’s around, triggers aren’t appropriate. Doing this helped me greatly.
● Doom Loops
Some see glimpses of a doom loop, where you’re entrapped in some hell loop you can’t escape. For some people, this is just an illusion of the paranoid mind returning online.
You can break such loops with a single act of free will, including acting against it. Make a choice, any choice, and it’ll cease to exist. We are creatures of free will (debatable), but all that’s needed is one choice to not participate in that loop, and you will no longer see it in front of you.

● Patches and Upgrades

When you undergo ketamine therapy, your neural networks collapse and reset – through the example shown with the sheep.
When this happens, the mind is rebooted, collapsing brainwaves and neural networks. Many report witnessing the act of this reboot as it happens, and it gives the impression that recent updates and patches were applied when it happens.
This experience is not unique – it comes reported by several.
It’s analogous to your PC needing a reboot to install patches. When the brainwaves recover and neural networks come back online, they come back in no predictable order, and as a result, you will form new relationships in your brain. New dendrites grow, as do synapses, and maybe they need programming to do so.
Regardless, you’ll appreciate the mental clarity you get from recently recycled networks. And the new points of view.
I know It sounds odd, especially to someone completely new to ketamine. But once experienced, it is quite an apt description.
● Dosing Levels
See: Dosing
See: Non-Ordinary States of Consciousness
Dosing is particular to the individual, so please talk with your provider about low, intermediate, and high doses for your body weight. I will not share my dosing as I do not want it to be generally applied.
Quick Dosing Levels and Effects
Overall, though, I advocate for higher dosing up to a point — near the top end of dosing, you become incoherent and can khole, which is ego death. Bipolar type 1 people run the risk of brief psychotic episodes. I don’t think this is productive, and it can be traumatic, which should be avoided due to the perineuronal network being down.
Below this, however, is coherent dissociation, which I find most therapeutic. This level separates my mind from my body and lets me comprehensively analyze my memories and stimulus-response patterns.

There is controversy in research around therapeutic doses. Some research indicates the therapeutic value in going through a ‘k-hole’ experience, while others have shown therapeutic value without that being necessary.
Some research shows ketamine disconnects a hyperconnected default mode network that ruminates, and it is unclear what dose is required to do that.
There is also the formation of new synapses and dendric spines in areas damaged by maladaptation 12-72 hours after dosing, which is also hypothesized to create some of the therapeutic effects – and in that case, it’s not required to wipe your cognition, ego die or ‘k-hole’.
So, while I think moderate doses to promote disassociation are helpful from a PTSD & CPTSD perspective (untangling triggers and divorcing the mind from the stimulus-response), it isn’t clear how high a dose is required to solve depression and regrow the synapses damaged by depression and maladaptation.
Again, studies have shown that ketamine takes down the perineuronal network, which protects the brain against trauma. Knowing this, it’s essential to ensure that the ketamine experience doesn’t traumatize you. At high doses, especially without any prior experience with ketamine, a khole (ego death) can be traumatizing. The lack of coherent thought and inability to remember yourself or aspects of your life can be scary.
For this reason, I recommend you start low and slowly work your way up in dosing, ensuring you stay within your comfort zone throughout treatment. This may result in smaller increases in doses than recommended or additional doses to reach the level of disassociation you find therapeutic. Many people have reported (and research is showing) that moderate dosing is very effective.

Make sure you communicate with your provider actively while undergoing the experience. They can vary as you go by speeding, slowing the drip, or increasing or decreasing the total dose. If you feel concerned, anxious, or panicky, contact them immediately so they can slow it down for you. Do not traumatize yourself – as you work up in doses, the anxiety around the experience will lessen, so you can work up to the higher intensity if you wish but go there on your terms. If you find yourself in a place you aren’t comfortable, speak up – you are in complete control.
Here is an excerpt of a conversation with a Reddit user, u/awkwardflea, who advocates for comfortable, mid-level dosing so you can get an idea of what it looks like.
“I started at 0.5mg/kg but decided to try upping the dose a little because I was emotionally overwhelmed. It was like exploring an inner dreamscape, but I didn’t have the emotional regulation skills to process everything that was coming up. Someone on here suggested that I might be a little more comfortable with a little more distance. However, I still found 0.5mg/kg helpful in gaining insights and processing trauma. I felt terrific afterward, though. Happy and grounded after the first infusion.
At first, I tried upping it to 0.6mg/kg, which was a disaster. It became increasingly intense and a giant looping flashback of a traumatic event. I had enough control at the lower dose to bring in a friend or affect my experience. At 0.6mg/kg, I was just stuck. I didn’t get the same insights or symptom relief as I did at 0.5mg/kg.
My most helpful infusions (at 0.55mg/kg with magnesium over 40 min) were like exploring an inner dreamscape with safety and perspective. It wasn’t precisely revisiting past trauma but more like metaphorical visuals that gave me insights (watching my father drift away on a raft, seeing my mother frozen in time, passing through a portal, and turning into a bird with metal wings). It all made sense to me during the infusions or the integration work a few hours later. It was trippy but specific to my situation. I sobbed through most of my infusions and processed a lot. And the insights (e.g., I am more than what was done to me) felt like a light bulb turning on, like flipping a switch in my brain. I didn’t have to struggle to accept things I’d been working on in therapy forever; they just became true. I can still open my eyes and communicate at 0.55mg/kg; I don’t.”
For another view on the ketamine experience itself, read WhiskeyBravo’s story as he undergoes therapy and journals about his experiences.
Just be careful not to traumatize yourself, as those traumas are potentially severe with the perineuronal network being down.
● Maintenance & Boosters
See also: Maintenance & Boosters.
When using troches, I treated myself one week out of every five weeks. I did this to prevent bladder damage, allowing four weeks for healing. I also don’t want to be on ketamine all the time. I work in a highly intellectual field and could not have neural networks offline routinely.
For the first three years of my treatment, I used the at-home troches, taking high doses every other night, the equivalent of 4 IV experiences. I administered half the dose at first, then an hour later ¼, then an hour later ¼.
More recently (over the last two and a half years), I have done one 2-hr IV every 3 months for maintenance.
The weeks in between treatments are 100% remission. The main reason I still treat periodically is prophylactic. I am healthy and want to be proactive about staying that way. As you’ll read below about ‘Ketamine as a cure’ though, I’m at the point described, where I’ve ‘graduated’ from needing ketamine at all to feel better. I could just as easily spot treat, without fear of relapse of symptoms.
At 7+ years along now, my sessions are just a lovely 2-hour meditation and an excellent way to center me, and as a reminder every so often.

●Ketamine as a Cure

See: Ketamine as a Cure
Some report ‘graduating’ from needing regular boosters, and I have a theory about that. As ketamine builds the new healthy brain networks by adding synapses and dendrites, they start out weak. They need daily use and nourishment with repeated doses to grow out fully. Like muscles, you need to hit the mental gym to strengthen. With practice, healthy networks get enough reinforcement, and they become the dominant networks and replace maladaptive ones, which then atrophy.
It makes sense that the need for continued boosters becomes less necessary when the healthy brain network is dominant. There still might be the occasional trigger, or you may want to ‘prune’ your brain periodically to prevent Alzheimer’s, but monthly dosing is likely no longer necessary. You could, in theory, spot treat. Three years in, I looked over the prior year and decided I am at the point where my healthy brain networks are dominant, so I stopped at home troches and do one 2-hour IV every three months instead. I’ll post updates here as I learn more through the experiment.
Update: In years 4-5, I have settled into one 2-hour IV once every 3 months, 160mg/175lbs as maintenance, and have had zero recurrences of any symptoms I described above. The three-month window has been very successful.
● Ketamine and THC

See also: Ketamine w/Concurrent Recreational Drugs
Here, I cover THC, but this can be applied to most intoxicating recreational drugs.
THC during ketamine therapy is a controversial topic. Many of us, myself included, were self-treated with THC before ketamine.
Ketamine and THC interfere with each other, if not pharmacology, then mentally.
One of the most significant factors in ketamine therapy is the formation of new healthy brain networks through the growth of synapses and dendrite spines. For those to grow correctly, you need to train them and reinforce them. This must be done with as healthy a mind as possible for the best long-term effects.
If you’re under the influence of another drug, especially chronically, those networks form maladaptive and could worsen chemical dependency because they were trained like that. What should be a healthy brain network grows to be a chemically dependent one.
So, many providers recommend (and test) that THC not be present during treatment so those networks grow correctly. This is the right approach. That doesn’t mean you can’t imbibe some once you’ve grown out of the healthy net (mostly there after the series of six and a few boosters) but don’t train your new, healthy mind to be habituated on a drug.
There is good news here, though, ketamine makes quitting amazingly easy. It’s like it wants to. With one dose, you can stop, easy peasy. With the window of neural plasticity, you can decide to change a habit like that, and poof, like magic, it changes.
I know that’s not what some wanted to hear, and if they ask around, I’m sure they’ll find some that advocate THC while using ketamine. As I said, it’s controversial.
I quit THC personally, and now that my brain is healthy and reinforced, I also stopped drinking LSD, THC, DMT, mushrooms, caffeine, and several prescriptions that I no longer need. It turns out that baseline me is the version of me I like best. That’s a personal choice, of course, but I find my healthy mind is preferable to other altered states.
● Spravato vs. Racemic Ketamine
See also Spravato vs. Racemic Ketamine for additional detail.
Update: See this recent study, which proves across 3299 patients that spravato is significantly less effective than racemic ketamine.


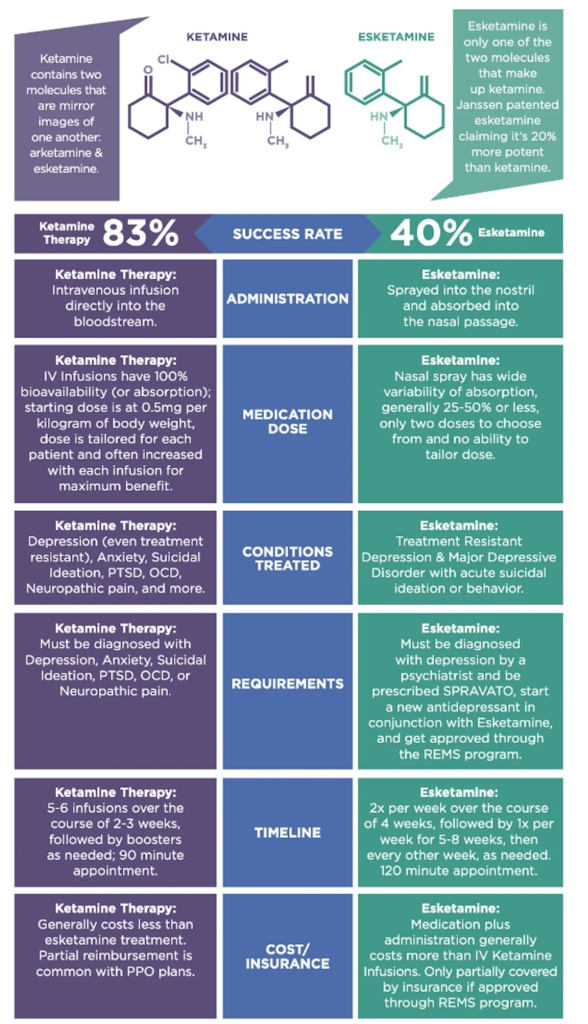
Spravato is esketamine aka the s-anomer of ketamine. Racemic ketamine is a mix of r and s isomers, targeting more receptors.
Advantages of Spravato:
- Clinically proven to treat treatment-resistant depression
- Approved by the FDA and VA for TRD treatment
- It can be cheaper than IV ketamine treatments
- It is often covered by insurance
- For some may be the only option – and it’s better than nothing
- Stronger disassociation than ketamine at equivalent doses
Disadvantages of Spravato:
- Not shown to improve cognition in limited testing
- Limited potential for dissociation
- It can be more expensive than ketamine troche, rapid dissolve tablets
- Limited dosing options per manufacturer recommendations
- Not shown effective, either clinically or anecdotally, for other mental illnesses than TRD.
- Nasal spray only
- Only approved to treat depression
Advantages of Racemic Ketamine:
- Flexible in form and dosage
- Available in more treatment centers
- No upper limit to disassociation dosages (they can be dosed more strongly)
- Cognitive benefits shown via correlated studies
- Treats a broader array of mental illnesses
- Some methods of administration are cheaper than Spravato
Disadvantages of Racemic Ketamine:
- Few clinical trials. Benefits are primarily shown through psychological tests and lots of patient and doctor reports.
- Limited backing studies
- Little FDA rigor
- IVs can be more expensive than Spravato
Note that dozens of people have done ketamine proper and Spravato, and they universally report that ketamine is far more effective across a broad spectrum of mental illnesses. A few (and clinical studies show) that Spravato is effective against TRD regardless of the cognitive or dissociative benefits. So far, only one person has reported Spravato being equally effective. I recommend trying ketamine if you have the option between ketamine proper and Spravato; ketamine will be cheaper, more flexible to dose, and by many reports, more effective across the board when people have taken both. Admittedly, though, it is largely anecdotal.
As studies proceed, I will add more info here. Spravato shows potential, and clinical evidence is sparse on the efficacy of racemic ketamine, whereas Spravato has more clinical evidence. Suppose you wish for a more reported effective path. In that case, racemic ketamine has more of a record of accomplishment and shows solid, consistent results for most across various mental illnesses. In contrast, Spravato has only been clinically proven for TRD and has few anecdotal reports of being effective in other mental illnesses.
Note that by way of comparison between IV ketamine and Spravato, especially if you have limited insurance coverage or are restricted by the VA, Spravato may well be the better choice and potentially cheaper. Choose your route of administration method carefully, as the costs vary, and Spravato is more expensive than many ketamine administration methods.
● Recommendations

See also: Session Recommendations
Music
Play instrumental music. Part of this is you want to let your mind wander, to associate and disassociate freely. Music with words prevents this because it constrains you to a topic.
- ‘Ketamine Saved Me’ (Spotify) – very few uplifting words here and there.
- ‘Ketamine Infusion // Heart Opening‘ (Spotify)
- ‘Infusion‘ (Spotify)
- This is Enigma (Spotify).
- Subnautica Below Zero Soundtrack (Spotify).
- John Hopkins University Playlist (Spotify).
Eye Mask
- You’re going to want to maximize your mind’s eye. Block light so you can see mental imagery better.
Headset
- Ideally, something noise canceling. Note, at times, ketamine music can become atonal. Not unusual.
Red and Itchy Eyes
- If you have red or itchy eyes afterward, use antihistamine eyedrops.
See: Itchy Eyes
● Ketamine Assisted Therapy
See: Ketamine Assisted Psychotherapy (KAP)
See: Integration Guide
I can be uncommunicative at a therapeutic dose, whether IV or troches. I have a therapist trained in ketamine therapy that I worked with, but I ultimately decided to work with her in sessions separate from the ketamine.
Ketamine is a drug therapy. It opens you up to yourself in unexpected ways. Part of my root issue was that I was beaten senselessly as a child. At an early age, I internalized that I was evil incarnate as it must be my very existence that I was being punished for.
Out of this came a self-persecution complex I recognized and overcame.
The bottom line, though, is I’m not even sure a therapist could have ever gotten to the root of that.
Ketamine opened me up to myself so that I could find it.

I have had times where I’ve been on lower doses of ketamine and talked through problems/traumas/events as they’ve come up, and interactively resolving the issues while on ketamine can be effective.
Lots of people have benefited from working with therapists alongside ketamine therapy. Reddit user u/awkwardflea said, “I got a ton out of doing integration works a few hours AFTER infusions. I know at least one other person with CPTSD on here who also found that beneficial and an infusion doc supporting the post-infusion integration work approach.
I never tried ketamine-assisted psychotherapy (KAP), but based on my experience with infusions, I don’t think I’d find it beneficial. Even with the lower dose, my experience is very internal. I would lose a ton trying to talk to someone during it. My ego is still intact, but it takes a backseat and lets my subconscious steer, if that makes sense, unless I open my eyes and try to fight the treatment.”
I agree with u/awkwardflea in terms of KAP. Even when in a coherent state, my mind is working so quickly and associating and disassociating so many disparate thoughts with each other, and delving into all the associations that underlie triggers, having to talk through it would get in the way – and that’s if I could hold my train of thought long enough to carry on a conversation.
Something important here to mention! PTSD patients have typical maladaptive behavior as a result of triggers. Learn about these PTSD maladaptive behaviors and work through them intentionally in your ketamine therapy.
Mindfulness is a valuable approach in addition to therapy. Do a body scan several times daily, walk your senses, and take in the now as fully as possible. What does it feel like on your feet? How about the temperature of your skin? Can you hear anything? Your heartbeat? Can you see anything? The wind on the leaves? Soak in your surroundings and wire up those new synapses and dendrite spines to your senses as fully as possible. You’re rebuilding a healthy brain network; the more use, connection, and reinforcement you can give it, the better the long-term effects will be.
Watch this short video for an entertaining quick view of mindfulness and how to go about it.

● Contraindications
See also: Contraindications for a more comprehensive list.
Serotonin Syndrome
It has little on it, but in a singular case study, it was correlated with the concurrent administration of fluoxetine. Extremely rare, but be aware of this medication’s contraindications.
“For Ms. O, we suspected that administering ketamine in conjunction with
fluoxetine, 40 mg/d, led to serotonin syndrome. “
Lamictal and Risperidone
Both potentially reduce the effectiveness of ketamine, according to this study: Ketamine and other depression meds.
I take both, and ketamine still worked 100%, but I need higher doses than others.
The interaction between lamotrigine (Lamictal) and ketamine is not fully understood, and the available literature provides mixed results. Here are some key findings from various studies:
- A study titled “Modulatory Effects of Ketamine and Lamotrigine on Cognition: Emotion Interaction in the Brain” suggests that the effects of acute ketamine challenge are sensitive to modulation by pretreatment with lamotrigine, which inhibits glutamate release. However, the inhibition of glutamate release by pretreatment with lamotrigine did not influence ketamine’s subjective effects source.
- Another case report titled “Failure of ketamine anesthesia in a patient with lamotrigine overdose” discusses a situation where ketamine failed to work as an anesthetic in a patient who overdosed on lamotrigine. The authors suspected an interaction between lamotrigine and ketamine, as lamotrigine reduces the glutamate release needed to mediate ketamine’s dissociative effects source.
- A systematic review titled “Pharmacodynamic Interactions Between Ketamine and Psychiatric Medications Used in the Treatment of Depression” found that two out of five studies on lamotrigine indicated that the effects of ketamine were attenuated source.
These findings suggest that lamotrigine may potentially alter the effects of ketamine, possibly by inhibiting glutamate release. However, more research is needed to fully understand this interaction’s nature and implications.
Grapefruit Juice
There are reported interactions (as is common with grapefruit juice and other meds), but the exact effect caused is unclear.
Liver Interaction
- Rifampin, a tuberculosis drug that decreases ketamine
- St John’s Wort is a popular supplement for a variety of conditions that decreases ketamine
- Ketoconazole, an anti-fungal drug that increases ketamine
- Cimetidine (Tagamet), an acid reducer for heartburn and peptic ulcers that theoretically increases ketamine
- Orphenadrine (Norflex), a muscle relaxant, inhibits CYP2B6 and slows the breakdown of ketamine which increases the amount of ketamine in the body
- Dexamethasone, a common steroid, induces CYP2B6 and speeds up the breakdown of ketamine. This decreases the amount of ketamine left in your system to work.
According to more recent reports, rapamycin appears to be a catalyst to ketamine, prolonging its anti-depressant effects. There are very few studies in this area – so make sure you look this up and speak with your provider about it, as it may be a way to improve the effectiveness of your therapy.
In recent studies, ketamine has been shown to suppress aspects of the immune system. This is important because you may want to avoid sessions while sick or chronically ill.
Ketamine and benzodiazepines (benzos) both have central nervous system depressant effects, so using them together can lead to enhanced sedation and respiratory depression. This increases the risk of unconsciousness and potentially overdose.
Gabapentin and ketamine appear to by synergistic, with some reporting improved results when used in combination with one another. It has also been noted that they exacerbate side effects, however.
● Ketamine and Psychosis
See also: Bipolar 1 & 2
See also: Ketamine and Psychosis
While ketamine works very well in bipolar patients, those with psychotic features must maintain their antipsychotic while undergoing ketamine therapy.
Ketamine does nothing to solve psychosis and mania (I learned this firsthand), so keep using a mood stabilizer such as Lamictal and an antipsychotic such as risperidone.
High doses of ketamine can trigger short psychotic episodes during the peak in predisposed individuals, which indicates doses should be controlled (lower and longer, and/or lower and more frequently) for those with psychosis or schizophrenia.
That said, this study shows that ketamine is well tolerated in patients with a predisposition to psychosis and does not exacerbate psychosis more generally.

● Ketamine Cystitis (Bladder Harm)
See also: Ketamine Cystitis (Bladder Harm)
Note, like much around ketamine therapy, this section is controversial and the most often criticized. Do your research and know my guidance is quite conservative, according to many. The way I see it, since the risk here is long-term damage to the body, it is much better to be safe than sorry, so I am conservative intentionally.
Most chronic bladder damage seen with ketamine results from abuse in recreational users.
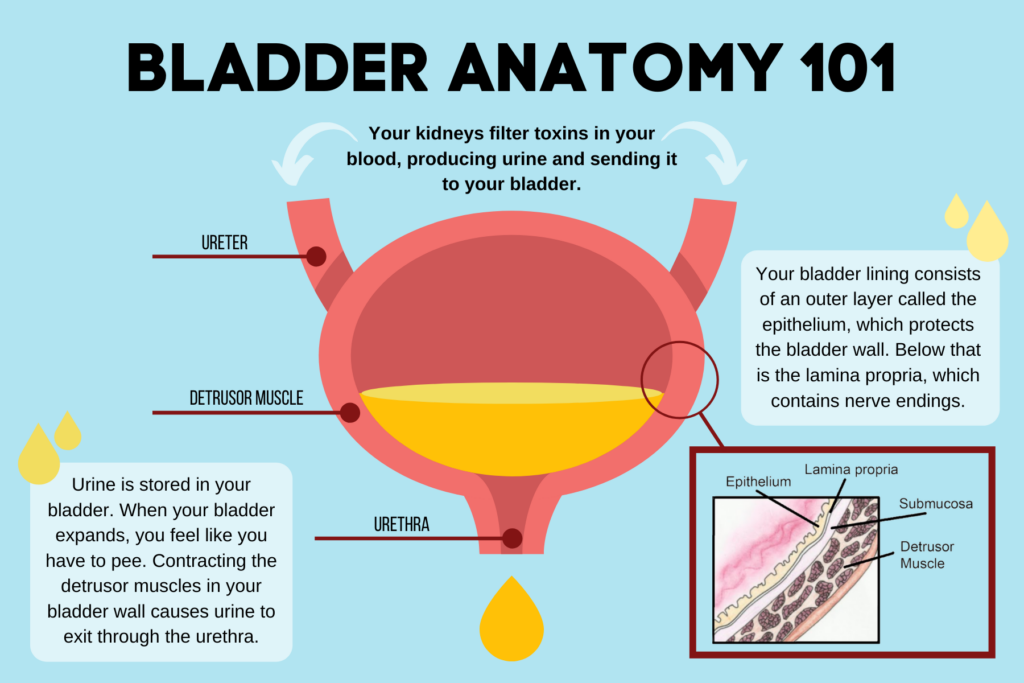
Bladder damage potentially occurs from chronic exposure to ketamine metabolites, which damage the inner mucosa lining of the bladder. There may also be damage to interstitial tissue, microvascular changes, and autoimmune responses. Chronic contact with metabolites is hypothesized to result in submucosal edema, vascular ectasia, detrusor muscle inflammation, and fibrosis. Collectively, this is called ketamine cystitis (KC). Lower urinary tract symptoms were found in around 30% of ketamine abusers.
I’m told dosing at 200 mg a day, and lower has been shown to result in extremely low (no) incidents of KC. If your dose exceeds 200 mg daily for over a few days, consider a break to allow the bladder’s mucosal layer to heal.
The bladder’s internal lining is made out of exactly the same tissue as the inner lining of your cheek. Ketamine crystals and metabolites scratch away mucosal membranes. This is why troches and RDT can often cause a sloughing of cheek cells. Just like your cheek, the bladder can heal the mucosal membrane within it completely as long as it doesn’t become too damaged. KC begins when ketamine crystals and metabolites scratch the mucosal membrane so much that it becomes worn away and exposes the tissue underneath. Ketamine metabolites also damage the underlying tissue, but unlike the mucosal membrane, the underlying tissue can’t heal. By taking a break early and often, the bladder heals between sessions, preventing the long-term symptoms of KC.
See: Bladder Health and the Mucosal Layer
This amount taken varies by the route of administration, based on its bioavailability. IV and IM are the most bioavailable forms, so lower relative doses in those forms result in the same therapeutic value as higher doses in other forms. For example, 200mg of troches may only require 50mg via IV. For those experiencing or prone to bladder issues, using more highly bioavailable forms may mitigate the risk of KC onset.
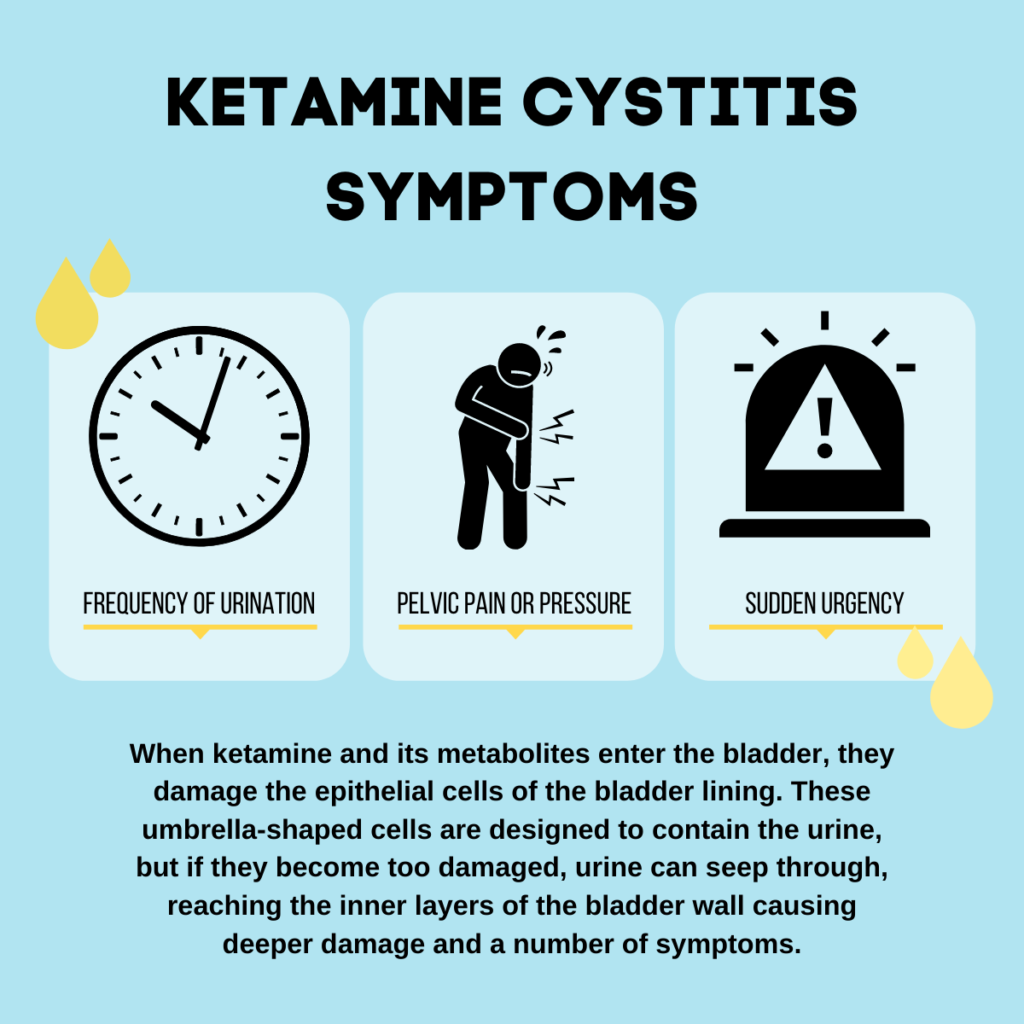
Trends toward KC damage can be monitored interactively – signs of progression toward KC are bloody urine, cloudy urine, increased urinary frequency, urge incontinence, bladder pain, and dysuria (burning). If you find these early signs, taking a break is safest. The bladder can heal itself completely early on, so those symptoms should clear up within a month if caught early.
Outside of active bladder harm management, drinking a lot of water is recommended, diluting the ketamine metabolites and reducing potential damage. Drink a lot of water after your session, not before, as it’s unpleasant to get up to pee while in the middle of a dose.
Additionally, even though KC is not well understood, potential treatment programs may be available, and research in this area shows the potential to reverse chronic long-term symptoms.
“Treatment with the antifibrotic compound N-acetylcysteine alleviated the symptoms and pathological characteristics of KC, indicating that the antifibrotic capacity of MSC therapy underlies its benefits. Thus, this study, for the first time, shows that MSC therapy might help to cure KC by protecting against tissue fibrosis in a KC animal model and provides a foundation for clinical trials of MSC therapy.”
● Disclaimer
See also: Site Disclaimer
Ketamine therapy can, at times, be challenging. Ketamine is not normally euphoric. Sometimes, subjective experiences with ketamine aren’t fun. Those sessions can be the most therapeutic, though. Whether it is a positive or negative experience, it benefits your psyche. The regrowth of healthy new synapses and dendrite spines will happen no matter the subjective experience.
Ketamine yields no results in 20% of people. I have read firsthand accounts of it not working. However, it worked great for me, and 80% of people responded well.
I am not a Dr, nor are the site collaborators. Dozens of providers have proofread us, and many use us as their patient primer, but nothing in this guide (or site) is to be taken as a substitute for legitimate medical advice from a qualified provider. This content is for informational purposes only. Ketamine research is constantly ongoing, and while we strive to keep current with recent advancements, our information may not always reflect the most recent study results. As a result, independently verify information through the sources provided and/or Google searches to ensure you review the most recent developments. Always consult a qualified provider about any changes to your treatment plan.
● Feedback
Please score us! We like to know how we’re doing.
● Questions & Comments

Please take a moment and consider the mind that made this site. It is healed perfectly.
If there’s anything I can do, ask. I love making a difference in others’ lives just as much as others love making big differences in my life. I do this to pay it forward.
You are welcome to post comments for me below, DM me on Reddit, or email the address on our About Us page.
Please fill out our 30-Second Success Survey. It aims to legitimize ketamine therapy in mental health further.



This is an amazing write up, thank you!
Of course, glad you enjoyed it 🙂
Excellent write up – very helpful. I’d like to ask if you’ve a couple of questions if I may. Have you heard of anyone getting a rash from ketamine? Also, have you heard of any benefits of taking Lion’s Mane mushrooms to help create new neural networks?
I have not heard of rash as a byproduct of ketamine, although it’s a risk with lamotrigine – so lamotrigine requires a slow titration up to mitigate that risk. Ketamine can cause a histamine response though, so take a Benadryl and have anti-hystimine eyedrops on hand to experiment to see if that helps.
As for mushrooms, I’m not familiar with Lion’s mane in general, but psychedelic mushrooms have been proven to be neurogenic. I asked ChatGPT about Lion’s Mane specifically, on your behalf, and it indicates that Lion’s Mane have the same properties:
“Lion’s mane mushrooms (Hericium erinaceus) are known for their potential cognitive and neurological benefits. Some studies suggest that they may have neurogenic properties, meaning that they can promote the growth and development of neurons in the brain. These mushrooms contain bioactive compounds called hericenones and erinacines, which are believed to stimulate the production of nerve growth factor (NGF), a protein that is essential for the growth, maintenance, and survival of neurons.”
Thank you for writing all of this! Very helpful and will aid me in my continued journey.
I take adderall Xr. Up until about a month ago I struggled with taking very high doses, not to get high, but because of debilitating exhaustion. Then I found out I have sleep apnea- and ever since I’ve been able to be much better about taking it as prescribed. I still occasionally take too much but typically because I’m trying to motivate myself out of depression. I have experience with taking LSD a few times, as well as mushrooms. I always noticed an immediate reduction in my depressive symptoms. Was able to reframe my thinking much easier. This was all before the high doses of adderall/some of them before I took it at all. The last time I took mushrooms was about 2 years ago, and I was on a normal amount of my adderall (since it’s XR it’s usually in my system anyways) – but the experience was so incredibly different it made me question the damage I’ve done to my brain / dopamine / etc. The entire experience was dark and scary and I could find no meaning in it (most of my trips have been uncomfortable because they’ve helped me process trauma) but this time was awful. I’m not scared of having a bad trip, I feel very comfortable with my ability to work through them – but I was wondering your thoughts about adderall and ketamine. I imagine I should try to wait until it’s completely cleared from my body to take ketamine because trying to process trauma and let your subconscious work with an adhd med in your system seems counter productive ? / if ketamine can still help my brain possibly heal from abusing it in the past. I apologize this is so long, but that mushroom trip was 2 years ago, and the reason I took them was to try to help myself process what was going on with me, and since my depression has been rapidly worsening.
Thank you so much for your time and this guide! You are truly wonderful!
You’re welcome with the guide; glad you found it helpful 🙂
So first, Adderall. I take Vyvanse, which is kind of like Adderall xr. It’s a stimulant, but it lasts 12 hours and does hepatic metabolization – meaning it gets processed by the liver with an enzyme that delivers the active ingredient incredibly smoothly all day (with no ups and downs). Both Adderall and Vyvanse active ingredients are stimulants. They are slightly different in amphetamine.
So in stimulants, we’re similar.
I did discontinue the Vyvanse when first starting ketamine therapy to see if I still needed it given the ketamine therapy. It turned out I did still need it. Ketamine therapy hadn’t solved my ADHD (so not trying to pull myself out of depression like you, though, more a focus and get things done need for me). Ketamine didn’t worsen those problems, but the ADHD persisted even with the ketamine. So I had to keep taking the stimulant and still do.
I think you’ll want to start low, and ketamine trips can be good or can go wrong, just like any other psychedelic. Subjective experience doesn’t matter, though. The magic is in the brain’s regrowth which happens regardless of the experience, it seems. Regarding brain damage that’s occurred by Adderall (which I doubt there is any), I think you’re right in that it would likely be repaired by the neural growth you get through your ketamine series.
For me, the sense of lack of depression I had with mushrooms came transiently at first, then more so, over time, has become permanent, in that I do 1 IV every month (2 hr) and have had zero recurrences of any of my original symptoms for over two years (since I wnt to using this booster regimen).
Thank you SO much. I had my first appointment this morning and my prescription is in the mail. I didn’t know you had answered I just happened to be reading through your guide again haha. You have no idea how happy I am to hear that you take Vyvanse, ever since that mushroom trip I was a little convinced I broke myself / wouldn’t be able to have the same therapeutic effects during a trip (although the more I learn about Ketamine it’s so different, but I was still worried haha) I definitely did abuse the hell out of my dopamine system (would wake up and take 90 mg Xr adderall, take another 60 Xr midday, take another 60 Xr a little later ~ ultimately decide to pull an all nighter and ingest another 60 xr / often (always always) intentionally combined with alcohol) ~ but I’ve been much better about it lately. I actually had a similar thought about seeing if I still need it, because I’m pretty sure I do but my ADHD seems to have its roots in trauma. I encounter a trigger, my brain runs the other way, I find myself doing something else haha.
I’m rambling a bit but just genuinely thank you! I’m going to try work tomorrow without my adderall/try taking my first ketamine dose this weekend to see how it feels. But you reminded me of something so important which is that the ketamine will be doing it’s work in the background regardless.
Thank you again ❤️ looking forward to starting this journey with your guide in hand haha.
Yeah, so what I found helpful with the Vyvanse is an accountability buddy. She puts a Vyvanse out every morning, and she keeps the bottle hidden, so I’m never tempted to go on a bender.
I’m glad you are all sorted on the ketamine front, and you should look forward on the trigger front. You can get rid of those completely. Amazing new world, going to be life-changing.
Hello, on Joyous 120mg oral daily, is bladder damage likely?
120mg is below the threshold for bladder damage as I understand the limits. Always be aware of the potential symptoms of KC, but as long as you don’t see anything I wouldn’t worry about it. 200mg a day is generally considered safe, in so far as I know (and I am not a Dr)
Hello, thank you for this write up, I have a consult tomorrow morning. I was wondering if you could expand on this section?
“Once the healthy synapses grew, I reinforced them. As I was triggered, I broke down trauma underneath and differentiated it from my new reality, rewiring them to no longer fire”
Are you talking about doing therapy in conjunction with the ketamine or is are you referring to just what happens while you are under the influence of the ketamine naturally? Does it help to prepare for the session with things you’d like to address or old traumas to revisit? Do you get more benefit from therapy alongside the treatment to reduce maintenance dose or move away from it all together? CBT, Somatic?
Well, it’s just kind of the way ketamine works. You can definitely take in triggers to work on, but the neural activity is independent. You will lose some coherency during the experience, so don’t beat yourself up if you don’t get to what you wanted to up front. Sometimes ketamine works in mysterious ways, so just relax and let it take you where it wants you to go.
Thank you! I love you. ❤️
Same back at ‘cha. Big virtual hug 🙂
Hi! This is in incredibly helpful, thank you. However, under the Contraindications section, there are 2 separate discussions about gabapentin, and they appear to be contradictory.
Thank you for the catch. There was earlier information, and then newer information, where the consensus had changed based on research and personal accounts. So I removed the older info.
Also appreciate the positive feedback!
I can’t tell you how grateful I am for this guide! I just started at-home ketamine troches and found this incredibly helpful. It’s extremely well put together! Do you have thoughts or resources about the affects of caffeine and nicotine on ketamine efficacy?
Thank you for your gracious comments Emilee.
I don’t know about caffeine. I suspect that it’s counterproductive. A little probably doesn’t hurt much. E.g., green tea has some caffeine, but only half a cup of coffee. Because green tea is believed to be highly prophylactic for ketamine cystitis and I use quite a lot of ketamine, dosing 5+ days a week, I’ve largely switched from coffee to green tea. I suggest you consider doing so yourself. And I certainly wouldn’t use any “energy” drinks that are very high in their caffeine content.
I have read that nicotine interferes with sublingual absorption. Not specifically for ketamine; rather, generally for all sublingual drugs. It goes without saying that smoking is highly injurious to health. So, stop smoking. Now then, you might be using a nicotine patch to help you stop smoking. So, your question might be predicated on that use of nicotine. You have to make a choice: try to quit cold turkey or take a chance that the nicotine from your patch might interfere with your ketamine therapy. My choice would be to take that chance.
Regards
IbizaMalta